Informed Consent, This Great Unknown

Informed consent is one of the main tools in psychology that professionals have to ensure their ethics and morals. Consent can even be considered as a process of bidirectional dialogue between patient and health specialist, without any physical document, or a term or contract. In the dialogue or document, the benefits and possible advantages derived from a treatment or psychological study are exposed.
Its formal definition ensures that consent was given freely and voluntarily by the research subject or patient for all that action in the health field, and that after receiving all the appropriate and necessary information, he evaluated the options for the situation and chose that one.
Its post-war origin
Perhaps you’ve heard of Josef Mangele, also known only as Dr. Mangele or Angel of Death. He was a German physician, and made history for his sadistic characteristics and terrible cruelty. Supporter of Nazism, he carried out experiments throughout the regime using human beings, especially newborn twins. He employed procedures that could involve pain, non-reversible physical and psychological damage, and that could even lead to death in some cases.
The history of informed consent therefore goes back to the end of World War II, then the second half of the 20th century. More specifically, its origin comes from judges in the city of Nuremberg. Proceedings that went through the judiciary in that city established sanctions for a large number of leaders, officials and collaborators of the Hitler regime, condemning them on war crimes charges.
Thus, from 1947 onwards, consent came to be considered a basic pillar of scientific research with human beings. In this context, North American physicians Leo Alexander and Andrew Comvay Ivy created a manual with a series of ethical standards entitled “Permitted medical experiments”. Later, this code would be called “The Nuremberg Code,” and his main point was the concern with the voluntary consent.
Informed consent content
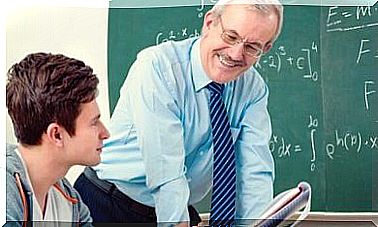
The psychology professional’s obligations are the user’s rights, and at the same time the user’s duties are the psychologist’s rights. Therefore, it is the professional’s obligation to inform the patient in a clear, rigorous, complete and truthful way about the content of the study, intervention, treatment or psychological research in which he will be a participant. But what then should be informed?
- Disorder assessment : inform the patient of the detected alteration or disorder.
- Nature and duration of the proposed treatment: number of sessions, follow-up, evaluation…
- Likely risks, side effects and inconveniences : These dangers are the most likely, based on scientific research.
- Expected benefits.
- Possible alternative treatments.
- In addition, it is currently also customary to add one more element: contractual aspects such as fees, situations that are covered, confidentiality limits and the possible participation of other parties.
Informed consent conditions
Informed consent is the formal medical and psychological procedure that seeks to respect the principle of patient autonomy. And, therefore, also his dignity. It refers to the obligation to respect everyone as a person and their preferences regarding the medical care they will receive. Taking into account the content of the document, the requirements that are necessary to give informed consent are listed below:
- Volunteering : is achieved without external pressure. That is, the person must give their consent in a free and informed way, without any pressure, force, fraud, deceit, persuasion, manipulation, coercion or any other way to obtain consent in an altered form. For this, the necessary time should be given for the patient to reflect, consult something or someone and decide.
- Capacity : the individual must have the ability to make decisions preserved. In other words, it has to be in full legal capacity to give consent. In this sense, there are situations in which this does not happen, such as changes in mental status, unconsciousness or minors.
- Information : the user must have sufficient information to be able to decide in the most rational and justified way possible.
- Comprehension : it is the psychologist’s job to ensure that the user understands all the information provided. Likewise, it is the latter’s right to receive it.

Written and oral
The information included in the document must be given in oral and written form. The aim is for the person receiving the communication to feel fully informed. Of course, after all this, the person must give their approval to the process. In the case of exclusively written communication, the process ends with the signature of the informed consent form. This signature confirms the understanding of all that has been communicated.
As seen, the informed consent procedure is fundamental in psychological practice. In addition, not using this communication mechanism can be a reason for professional sanction for psychological negligence.